COVID-19 has presented us with an opportunity.
Yes, it’s an unprecedented challenge, and our country has had to face dreadful horrors. But, it also brings us an opportunity to finally provide adequate, equitable access to healthcare for all. It also brings us an opportunity not just to save lives but also to create new livelihoods.
The key to both lies in telemedicine.
There are multiple benefits of expanding healthcare delivery through telemedicine. It can address the poor doctor-patient ratio, make high quality and specialised care available even in remote areas, and do it quickly and cost-effectively.
So, despite its apparent advantages, why haven’t we seen any significant success in telemedicine initiatives?
A successful telemedicine initiative will have to go beyond the paradigm of traditional healthcare. It is not simply a question of technology providing access to a ‘doctor’. If that were the case, telemedicine would already be a success because the technology has been around for a while. Patients, especially in rural areas, will require assistance while using telemedicine technology (where to look, where to speak etc.). Doctors may require translation assistance for local languages and dialects. Patients will require help understanding prescriptions and support post-consultation to follow recommendations. Receiving medical care without a physically present doctor is a significant shift, and patients will need help to build trust in the system.
Building trust in a system is a long term process. A process that depends on the system showing positive outcomes. And the key to building trust in telemedicine lies with the telemedicine service coordinator.
Enter the Telemedicine Coordinator
It is undeniable that telemedicine can significantly improve access, especially in rural and remote areas. But to achieve that potential, we need to envisage the role of a ‘telemedicine coordinator’.
In the field, a telemedicine coordinator mobilises communities through advocacy. They usually belong to these very same communities. They will interact with families in the village to check if people are reporting illnesses and what interventions are required. They will also have to spread awareness about health practices that curb the spread of diseases/pandemics. By addressing the community’s concerns, telemedicine coordinators make telemedicine more acceptable.
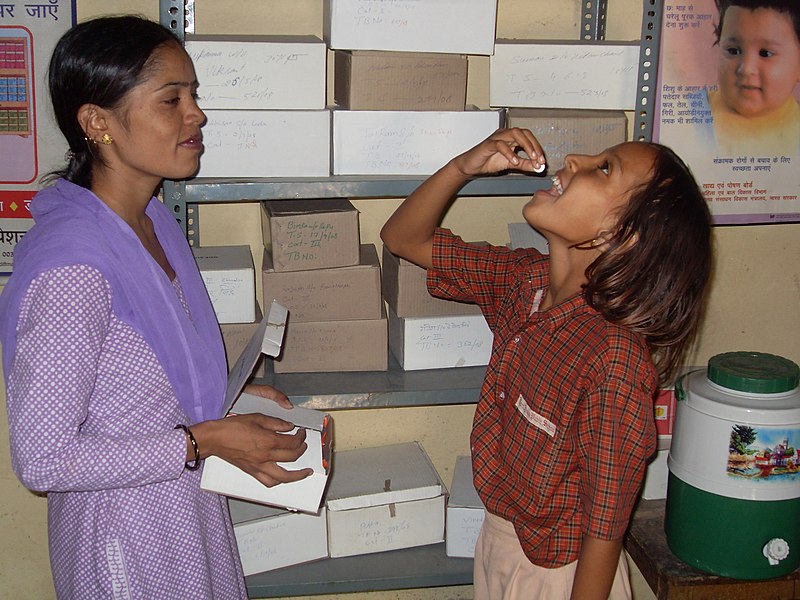
At the telemedicine centre, the coordinator is the first point of contact, makes a record of the patient details, understands the symptoms, and gives the doctor a concise briefing. It’ll be their responsibility to explain the treatment and prescription to the patient in detail, address any further queries, and facilitate follow up visits. A competent coordinator should understand the patients’ context, medical terminology, and enough about technology to enable a consultation.
Initiatives like the Aravind Eye Hospitals (65 million patients treated, 7.8 million surgeries) have a cadre of staff called patient counsellors. They play a critical role in ensuring treatments are patient-centric and that patients adhere to the treatment and regular follow-ups. Such a role can ease patients into a new system and fill gaps (language, technology, compliance to medication) in telemedicine.
Who becomes a Telemedicine Coordinator?
India has an extensive network of community health workers. The Auxiliary Nurse Midwife (ANM) is a role at the village level that links the community and health services. They work at the grassroots and are expected to be multi-purpose health workers. Their work goes beyond maternal/child health and family planning to health and nutrition education, environmental sanitation, immunisation to control infectious diseases, treatment of minor injuries, and administering first aid.
We need to upskill India’s 200,000+ ANMs to fulfil the role of a telemedicine coordinator and become the backbone of telemedicine in the country.
However, even in their current avatar, ANMs face challenges like low compensation, institutional support and social recognition. The training they receive is neither standardised nor adequate. There is no feedback mechanism or effective supervision that can help them improve upon their work. If this livelihood is to be developed, we must address these challenges and provide ANMs with a career growth path.
Empowerment and Accountability
ANMs have to be empowered to fulfil a higher-order role that increases their capabilities and income. As telemedicine coordinators, they will need skills to interact with the community at a deeper level. In addition, they must be enabled to operate with greater autonomy and accountability. Job security, social security, and insurance will give them financial safety and help them discharge their duties better.
We need quick interventions that can address these issues at scale.
Telemedicine can make a significant positive impact on the access, quality, and cost of healthcare in the country. The Covid-19 pandemic has allowed us to make a determined effort to take it forward. But for it to truly take off, we need innovations that develop the role of community health workers and solutions that make livelihoods more resilient and fill in the gaps to connect the last mile.
This article was originally written for Forbes.